Hip Joint – Bones, ligaments, blood supply and innervation |Anatomy|
We are going to be looking at the hip joint, its articulations, movements, blood supply, and innervation.
So, the hip joint is a ball and socket synovial joint, forming the connection between the lower limb and the pelvic girdle.
And the hip joint is also multi-axial meaning that it rotates on more than one axis. Which allows for a wider range of movement. Of course, the hip joint is designed for stability and weight-bearing.

The head of the femur articulates with the lunate surface of the acetabulum of the pelvis.

The lunate surface is concave, which is like the shape of a crescent moon as the name lunate suggests. And the hip joint can also be referred to as the acetabulofemoral joint.

Both the lunate surface of the acetabulum and the head of the femur are covered by hyaline cartilage. And hyaline cartilage is simple cartilage found on many articulating surfaces.
So, the acetabulum is the part of the pelvis where the ilium, ischium, and pubis bones merge and its concave almost entirely encompasses the head of the femur. Which contributes to the stability of the joint.

At the center of the acetabulum is a non-articulating surface which is known as the acetabular fossa. This part of the acetabulum contains loose connective tissue.

The acetabular labrum is the fibrocartilaginous collar or lip that surrounds the bony rim of the acetabulum and it bridges across the acetabular notch.

The labrum of the acetabulum increases the stability of the hip joint by deepening the acetabulum and increasing the area of articulation with the head of the femur.

The ball of the ball and socket hip joint is the rounded head of the femur. Which sits within the concavity of the acetabulum, which is our socket of the joint.
The head of the femur is entirely covered by hyaline cartilage except for an area called fovea capitis femoris.
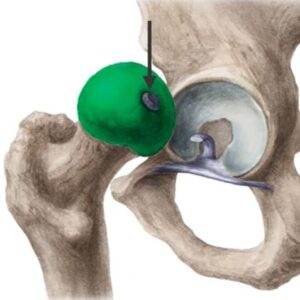
This is where the ligament of the head of the femur connects the femur at the fovea to the acetabular fossa, the transverse acetabular ligament, and the margins of the acetabular notch.

Capsule OF the Hip Joint:
So, the joint capsule of the hip joint attaches to the acetabular labrum and the transverse acetabular ligament proximally but is underneath the fibrous capsule.

The joint capsule is a strong fibrous capsule that can accommodate a wide range of movements and the capsule is strengthened and reinforced by the help of three ligaments.
Anteriorly and superiorly by the iliofemoral ligament, which connects the anterior and inferior iliac spine and the acetabular rim to the femoral intertrochanteric line. The iliofemoral ligament is the strongest of the hip joint ligaments.

Inferiorly and anteriorly, the pubofemoral ligaments arise from the obturator crest and the superior ramus of the pubis and blend with the capsule and the medial part of the iliofemoral ligament.

Posteriorly, the ischiofemoral ligament seen here from a posterior view connects the ischial part of the acetabular rim of the neck of the femur.

The fibers from the three ligaments are arranged in a spiral fashion around the hip joint which helps stabilize the joint by pulling the head of the femur medially into the acetabulum.
This reduces the amount of muscle energy required to maintain a standing position and prevents the hyperextension of the hip as well as excessive abduction.
Movements of the Hip Joint:
So the range of hip movement in the hip joint include
- Flexion – Movement of the leg forward
- Extension – Movement of the leg backward
- Abduction – Movement of the leg laterally
- Adduction – Movement of the leg medially towards the midline of the body
- Medial rotation – Internal rotation of the thigh towards the midline.
- Lateral rotation – Outward rotation of the thigh from the midline of the body.
- Circumduction – Conical precise 360degree movement of the leg.
Blood Supply of the Hip Joint:
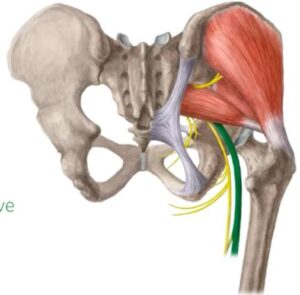
Blood is supplied to the hip joint primarily by the medial and lateral circumflex femoral arteries – the medial shown on the left and the lateral shown on the right. Both of these arise from the deep femoral artery.

And also by the artery to the head of the femur which runs within the ligament of the head of the femur which is shown in green and the artery to the head of the femur is a branch of the obturator artery.

Innervation of the Hip Joint:
(Green color indicates nerve)
1. Innervation of the hip joint comes anteriorly from the femoral nerve.

2. Inferiorly from an articular branch of the anterior division of the obturator nerve.

3. Poster superiorly from the superior gluteal nerve.
4. Laterally from the articular branch of the sciatic nerve.
For further advice do reach out to your local doctor or family doctor.
Do share this blog with your friends and family!





























