Tennis elbow: Causes, Signs and Symptoms, Diagnosis and Treatment
Tennis elbow is a condition characterized by painful inflammation of the outer part of the elbow. Also known as lateral epicondylitis.
Tennis elbow occurs when the tendons in the elbow become overloaded usually by repetitive motion of the arm and wrist. The pain is mostly located on the lateral side of the elbow but may radiate down into the back of the forearm and grip strength may become weakened.
About 2% of people are affected, it can pop up in people of any age but it’s more common in those who are 30 to 50 years.
Causes:
Tennis elbow is a type of repetitive strain injury that is caused by the repeated contraction of the forearm muscle
The specific forearm muscle that plays a role is the extensor carpi radialis brevis (ECRB) muscle. This muscle helps to straighten and raise or extend the wrist repetitive stress weakens the ECRB muscle, causing a series of tiny tears in the muscle’s tendon at the point where it attaches to the outside of the elbow.

Over time the tears damage the ECRB muscle leading to inflammation and pain.

Tennis elbow can be triggered by any activity that involves repetitive twisting of the wrist such as:
- Tennis and other racquet sports
- Golfing
- Swimming
- Turning a key
- Using plumbing tools
- Repetitive computer mouse use
- Frequently using hammer
- Painting
- Cutting up cooking ingredients, particularly meat
Symptoms:
Pain on the outer part of the elbow that is mild at first but gradually gets worse,
- A weak grip.
- Pain radiating from the outside of the elbow down to the forearm and wrist.
- Increased pain when shaking hands.
- Squeezing an object
- Turning a doorknob
- Holding a coffee cup
- Pain when lifting something or using tools
Diagnosis and Treatment:
Tennis elbow is usually diagnosed during a physical exam. The doctor will inquire about your job, whether you are into any sports, and how the symptoms developed. The doctor will perform simple tests to help make a diagnosis.
The doctor may apply pressure on the affected area or may ask you to move your elbow, wrist, and fingers in various directions physical examination and medical history are enough to make a diagnosis in most cases.
However, if the doctor suspects that something else may be causing your symptoms. The doctor may suggest imaging tests, such as an X-ray or MRI scan.
Tennis elbow often resolves on its own. About 80 to 95 cases can be treated with self-care measures.
During treatment, the doctor will first prescribe one or more of the following:
- Rest
- Ice pack
- Nonsteroidal anti-inflammatory medicine such as ibuprofen
- Physical therapy
- Steroid injection
- Ultrasound Therapy
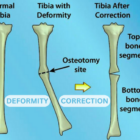
Surgery may be needed if symptoms don’t improve after six months or a year of treatment surgery may be performed through a large incision made directly over the elbow open surgery or through several small incisions. Both methods are employed to remove any dead tissue and to reattach healthy muscle to the bone a splint may be used to immobilize your arm after surgery to help restore muscle strength and flexibility.

For more information talk to a healthcare provider.
If you have any questions about Tennis elbow, please feel free and leave a comment.
Do share this blog with your friends and family!