A spinal cord abscess is a rare but serious condition where pus builds up in or around the spinal cord due to infection. This swelling puts pressure on the spinal cord and can lead to permanent nerve damage or paralysis if not treated early. It is most commonly caused by bacteria such as Staphylococcus and Streptococcus.
Who Is at Risk?
Spinal cord abscesses occur more often in people who:
◼️Use intravenous (IV) drugs
◼️Have weakened immune systems (HIV/AIDS, cancer, organ transplant patients)
◼️Have poorly controlled diabetes
◼️Experience frequent back injuries
◼️Have had spinal surgery or invasive spinal procedures
◼️Have infections elsewhere in the body
Common Causes:
Bacterial Infections
Most spinal cord abscesses are caused by bacteria, especially:
◼️Staphylococcus
◼️Streptococcus
◼️ Gram-negative bacteria may also cause infection, but less commonly.
Other Microorganisms
Rare organisms such as Actinomyces, Listeria, Proteus, Pseudomonas, fungi like Histoplasma capsulatum, and parasites like Sparganum can also cause abscesses.
Chronic Health Conditions
Certain diseases increase the risk, including:
◼️Tuberculosis (a major cause of epidural abscess in many countries)
◼️Crohn’s disease
◼️Infections spreading from nearby organs (e.g., ruptured gallbladder)
Symptoms:
Early stages may show no signs. As it progresses, symptoms include:
◼️Fever and chills
◼️Severe back pain
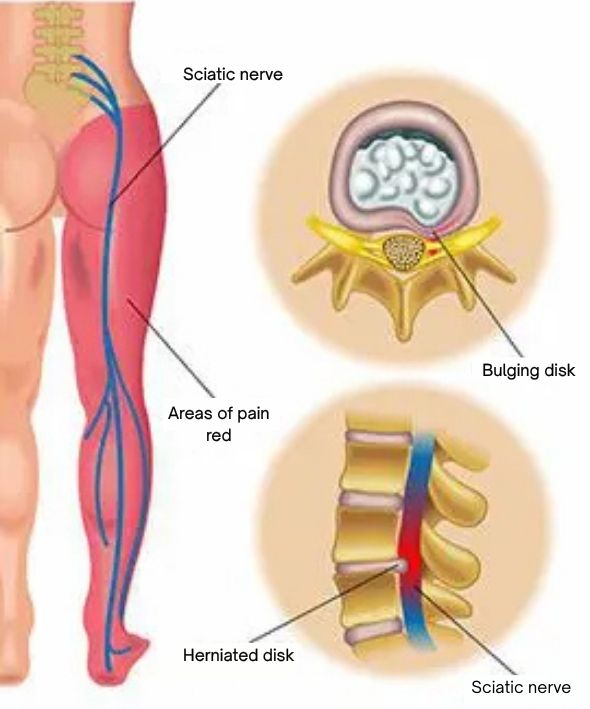
◼️Pain that spreads to the arms, shoulders, hips, legs, or feet
◼️Weakness or loss of movement below the affected area
◼️Loss of sensation or numbness
◼️Loss of bladder or bowel control
◼️Difficulty walking or paralysis in severe cases
For more information, talk to a healthcare provider.
If you have any questions about SPINAL CORD ABSCESS? Please feel free to leave a comment.
Do share this blog with your friends and family!