Lower back pain is a common issue affecting millions of women, often disrupting daily life and overall well-being. While it may seem simple, the causes behind this discomfort are diverse and sometimes complex. Understanding what triggers lower back pain can help you manage it more effectively.
Causes of Lower Back Pain:
◼️Stress & Anxiety: Emotional stress increases muscle tension and pain.
◼️Osteoarthritis: Wear and tear of spinal cartilage causes stiffness and pain.
◼️Muscle Strain: Poor posture, overuse, or sudden movement can trigger pain.
◼️Pregnancy & Childbirth: Added weight and posture changes strain the lower back.
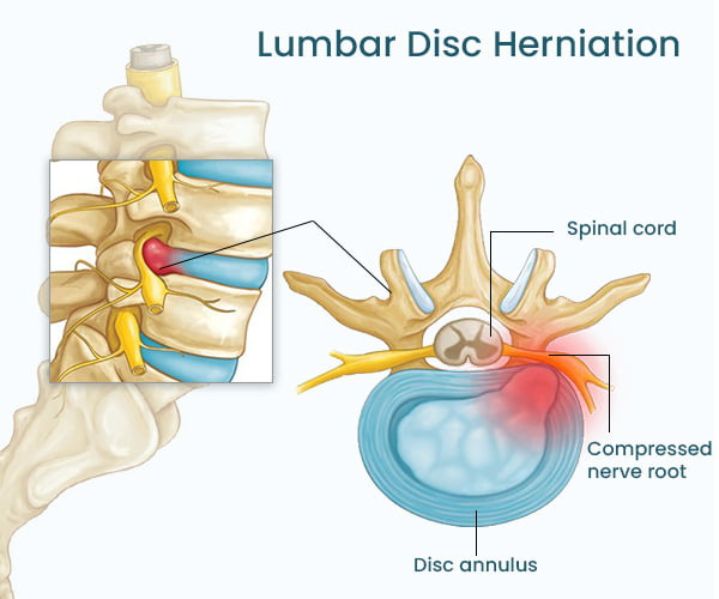
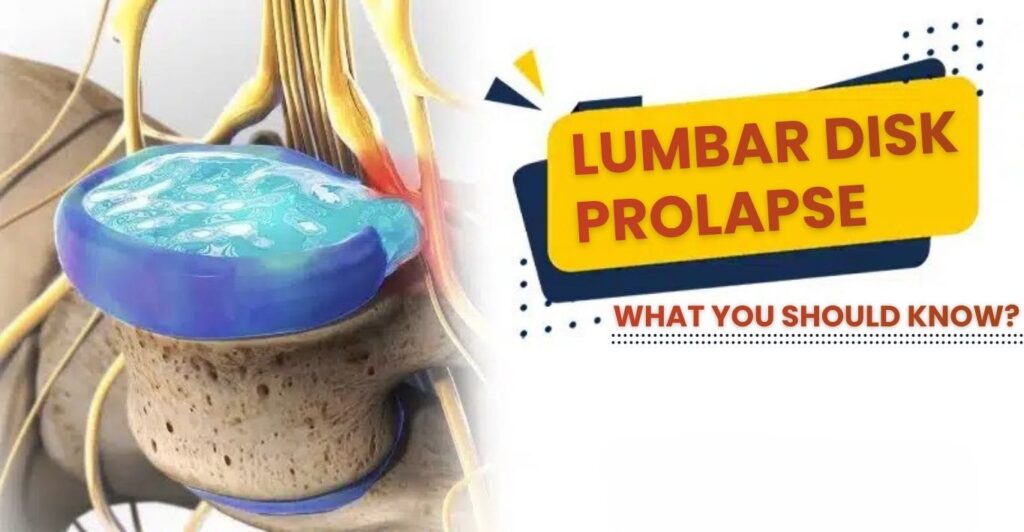
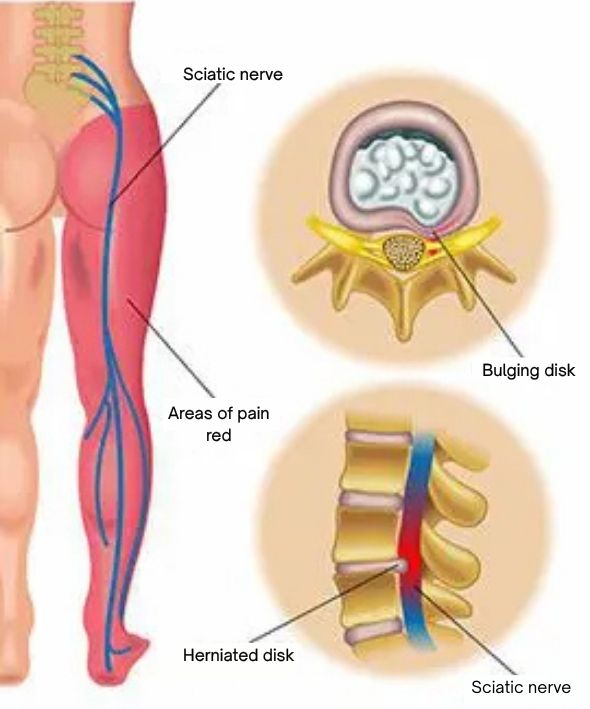
◼️Spinal Issues: Conditions like scoliosis, lordosis, or herniated discs cause chronic pain.
◼️Hormonal Changes: Menstruation, pregnancy, and menopause affect muscles and joints.
◼️Kidney/Bladder Issues: UTIs, infections, and kidney stones may appear as lower back pain.
◼️Gynaecological Problems: Endometriosis, cysts, fibroids, and PID can cause referred back pain.
Symptoms to Watch For:
◼️Muscle stiffness or spasms
◼️Pain when lifting or bending
◼️Pain linked to menstrual cycles
◼️Tingling or numbness in the hips or legs
◼️Limited ability to bend, move, or sit for long periods
◼️Persistent dull ache or sharp pain that may radiate to the legs
◼️Changes in bowel or urinary habits (seek medical attention promptly)
How to Manage & Prevent IT:
◼️Maintain good posture
◼️Use proper lifting techniques
◼️Apply heat or cold packs as needed
◼️Manage stress through relaxation techniques
◼️Exercise regularly and strengthen core muscles
◼️Seek medical advice if pain persists or worsens
For more information, talk to a healthcare provider.
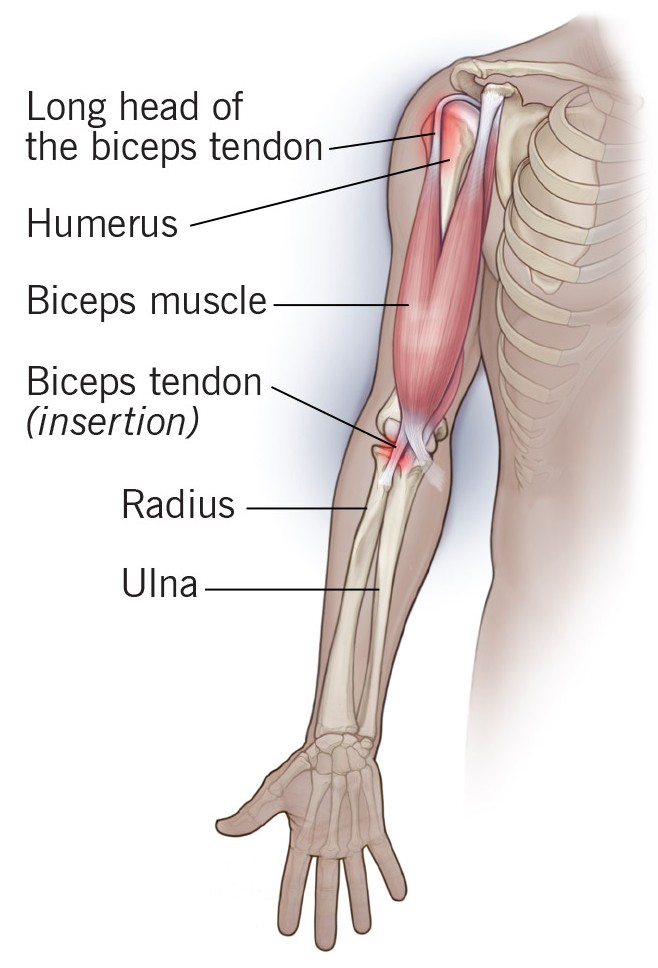
If you have any questions about SHOULDER INJURIES, Please feel free to leave a comment.
Do share this blog with your friends and family!