Fibula: Feature, Fracture Types, and Symptoms
The ankle is made up of three bones the tibia or shin bone, the fibula or calf bone, and the talus. The most common ankle fracture usually involves the fibula.
Side Determination of Fibula:
How do we determine the side of a fibula? The upper end of the head is slightly expanded in all directions. The lower end or lateral malleolus is expanded anteroposterior and flattened from side to side.

On the medial side of the lower end, there is a triangular articular facet anteriorly and a deep malleolar fossa facing posteriorly.
Features of Fibula:
The Fibula has an upper end, a shaft, and a lower end.

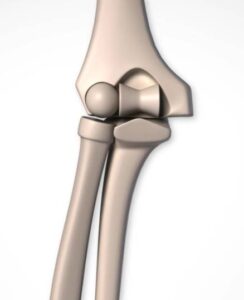
Now let’s look at the upper end of the fibula. The upper end is slightly expanded in all directions.
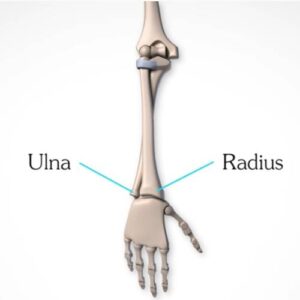
The fibula is the cylindrical lateral bone of the leg that is very small and thin. If you look at the placement of this bone which is parallel to the tibia. The tibia is the main part with the fibula acting as a pin that has to be inserted in the loop.
It is also called the calf bone because it’s present at the back of the leg. The fibula bone it’s not weight-bearing. The tibia is the weight-bearing bone of the leg.
The fibula is so non-weight bearing that it can be taken out of it and use if for bone reconstruction elsewhere in the body.
So its main functions are is forming the ankle joint. And a site of muscle attached as we have got lots of muscles attached to the fibula and the tibia and the interosseous membrane. So muscle attachments forming the ankle joint.
Basically, fibula fractures are very common, and fibular fractures commonly happen due to minor trauma.
The fibula is the lateral and smaller bone of the leg. It is very thin as compared to the tibia.
What are the types of fibula fractures?
Fibula fractures occur around the knee, ankle, and middle of the leg. There are types of fracture, which can also affect recovery and treatment. These types include:
- Avulsion fracture – a fracture in which a small part of the bone gets pulled off.
- Lateral malleolus fracture – a break around the ankle.
- Fibular head fracture – a break near the knee.
- Shaft fracture – a break that often affects the middle of the leg due to direct impact.
- Stress fracture – a hairline fracture due to repetitive injury e.g. Soccer, rugby, and snowboarding.
What are the symptoms of a fracture?
Other than pain and swelling, other signs of a fibula fracture include:
• bruising and tenderness
• deformity in the lower part of the leg
• pain that gets worse when putting pressure on the leg
• tingling or numbness, which usually happens if there is a neurovascular injury
Other joints and bones involved, such as the tibia.
Educational fibula fracture platting procedure:
First, the surgeon will make an incision over the fracture and a clamp (surgical tool) is used to hold the broken bone in place using special instruments a hole is drilled in the bone and a screw is used to hold the fracture in the correct position.
Next, the distal fibula plate is placed onto the bone and held with two pins then using special instruments screws are inserted through the plate to hold it onto the bone. After the ankle fracture has been fixed with a plate. Your surgeon drills holes in both the fibula and the tibia just above the ankle joint. The implant is inserted through the holes until it reaches the other side. Then your surgeon pulls back on the handle positioning the button against the bone.
Finally, the round button is placed against the plate and your surgeon pulls on each suture (Thread-like material) until the desired tension is achieved. This completes the ankle fracture repair.
We recommend you to take your doctor’s advice for proper guidance.
Do share this blog with your friends and family!