Understanding Deformity Correction: Techniques and Advances
Deformity correction is a specialized area of orthopedic medicine focused on realigning bones and joints to their proper anatomical position. Whether due to congenital conditions, trauma, disease, or growth disturbances, deformities can significantly impact an individual’s quality of life, causing pain, functional limitations, and aesthetic concerns. This blog aims to provide a comprehensive overview of deformity correction, exploring the techniques, processes, and advancements in this critical field.
What Is Deformity Correction?
Deformity correction involves the surgical or non-surgical realignment of bones and joints to restore normal function and appearance. The primary goal is to improve the patient’s mobility, reduce pain, and enhance overall quality of life. This process can address a wide range of conditions, including:
- Congenital deformities (e.g., clubfoot, scoliosis)
- Post-traumatic deformities (e.g., malunited fractures)
- Degenerative diseases (e.g., arthritis)
- Growth disturbances (e.g., limb length discrepancies)
Techniques In Deformity Correction :
1. Acute Deformity Correction :
Acute deformity correction is a medical procedure aimed at rapidly realigning bones or joints to their proper anatomical position. This procedure is often employed in the treatment of fractures, dislocations, and congenital or acquired deformities. The process involves several steps and considerations, which can be categorized into preoperative planning, surgical techniques, and postoperative care.
Preoperative Planning:
1. Assessment and Diagnosis:
- Imaging Studies: X-rays, CT scans, and MRIs are used to assess the extent and nature of the deformity.
- Physical Examination: A thorough physical examination helps to understand the functional impact of the deformity.
- Patient History: Medical history, including previous treatments and surgeries, is reviewed.
2. Planning:
- Correction Strategy: Deciding whether to use internal fixation (e.g., plates, screws) or external fixation (e.g., external fixators).
- Simulation: Computer-assisted simulations or models may be used to plan the correction precisely.
- Patient-Specific Considerations: Age, overall health, and bone quality are considered to tailor the approach.
Surgical Techniques:
1. Anesthesia:
- General or regional anesthesia is administered based on the patient’s condition and the procedure’s complexity.
2. Exposure and Preparation:
- Incision: A surgical incision is made to access the affected bone or joint.
- Soft Tissue Management: Careful handling of soft tissues to minimize damage and facilitate healing.
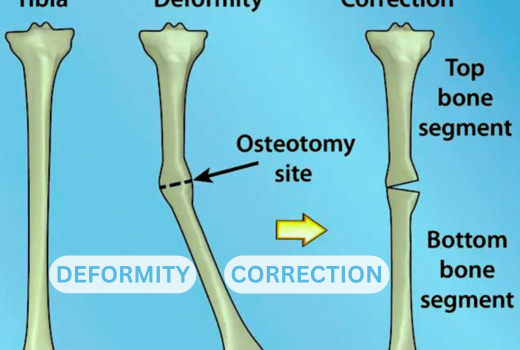
3. Osteotomy:
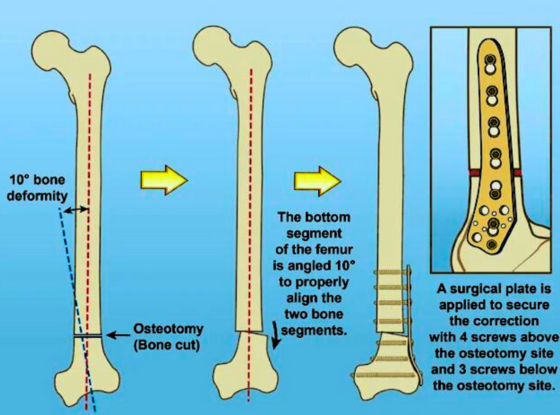
- Bone Cutting: An osteotomy (surgical cutting of bone) is performed to correct the deformity.
- Realignment: The bone segments are realigned to the desired position.
4. Fixation:
- Internal Fixation: Plates, screws, or rods are used to hold the bone in the corrected position.
- External Fixation: External fixators are applied to stabilize the bone from outside the body.
5. Adjustment and Verification:
- Intraoperative Imaging: X-rays or fluoroscopy are used to verify the correction.
- Adjustments: Fine adjustments are made as needed to ensure proper alignment.
Postoperative Care:
1. Recovery:
- Monitoring: Regular monitoring for signs of infection, proper healing, and correct alignment.
- Pain Management: Medications and other strategies are used to manage postoperative pain.
2. Rehabilitation:
- Physical Therapy: Initiated to restore function, strength, and range of motion.
- Weight-Bearing: Gradual progression in weight-bearing activities based on healing progress.
3. Follow-Up:
- Regular Check-Ups: Scheduled visits to monitor healing and detect any complications early.
- Imaging Studies: Periodic X-rays or other imaging to assess bone healing and alignment.
Risks and Complications:
- Infection: Risk of infection at the surgical site.
- Nonunion or Malunion: Failure of the bone to heal properly or in the correct position.
- Hardware Issues: Problems with internal or external fixation devices.
- Nerve or Vessel Injury: Potential damage to surrounding nerves or blood vessels.
Acute deformity correction requires a multidisciplinary approach involving orthopedic surgeons, radiologists, anesthesiologists, and rehabilitation specialists to ensure optimal outcomes. The success of the procedure largely depends on meticulous planning, precise surgical execution, and comprehensive postoperative care.
2. Gradual Deformity Correction :
Gradual deformity correction is a technique used to slowly and precisely realign bones or joints over time. This approach is typically employed for more complex deformities, including those resulting from congenital conditions, trauma, or disease processes like osteomyelitis or growth disturbances. The method relies on the body’s natural healing processes and usually involves the use of external fixation devices. Here’s an overview of how gradual deformity correction works:
Preoperative Planning :
1. Assessment and Diagnosis:
- Imaging Studies: X-rays, CT scans, and MRI are used to evaluate the deformity in detail.
- Physical Examination: A thorough examination assesses the functional impact and the extent of the deformity.
- Patient History: Reviewing medical history, previous treatments, and any coexisting medical conditions.
2. Planning:
- Correction Strategy: Deciding the method and timeline for correction. Computer-assisted planning and simulations are often used.
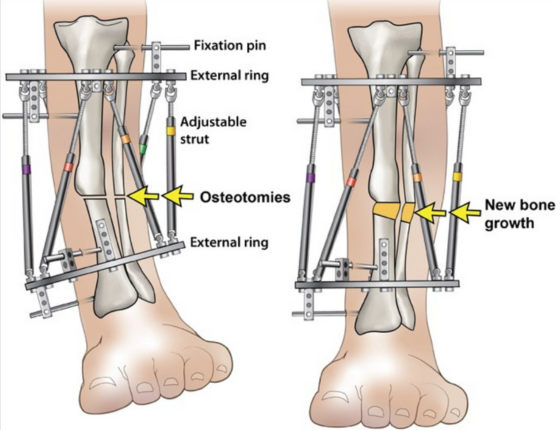
- Device Selection: Choosing the appropriate external fixator device, which can be monolateral, circular (Ilizarov), or hexapod-based systems.
Surgical Technique:
1. Anesthesia:
- General or regional anesthesia is administered to the patient.
2. Surgical Procedure:
- Incisions and Exposure: Small incisions are made to place the fixator pins or wires.
- Osteotomy: A controlled cut (osteotomy) is made in the bone at the site of deformity to enable gradual movement.
3. Application of External Fixator:
- Pin or Wire Insertion: Pins or wires are inserted into the bone segments through the skin and are attached to the external frame.
- Frame Assembly: The external fixator frame is assembled around the limb, connecting the pins or wires, allowing for precise control of bone movement.
Gradual Correction Process:
1. Distraction Phase:
- Initiation: Typically starts a few days after surgery to allow initial healing. The process is known as distraction osteogenesis.
- Adjustments: Gradual adjustments are made to the fixator (usually daily), moving the bone segments very slowly (approximately 1 mm per day) to correct the deformity.
- Monitoring: Regular follow-ups and imaging (X-rays) to ensure proper alignment and to adjust the correction as needed.
2. Consolidation Phase:
- Bone Healing: Once the desired correction is achieved, the bone is allowed to consolidate (harden and heal) in its new position. The fixator remains in place during this phase.
- Reduced Adjustments: Adjustments are minimized or stopped, and the bone is monitored for proper healing and strength development.
Postoperative Care and Rehabilitation:
1. Recovery:
- Monitoring: Close monitoring for signs of infection, proper alignment, and complications.
- Pain Management: Appropriate pain management strategies are employed.
2. Physical Therapy:
- Early Mobilization: Encouraged to maintain joint mobility and muscle strength, tailored to the patient’s tolerance and progress.
- Weight-Bearing: Gradual progression of weight-bearing activities as allowed by the surgeon.
3. Follow-Up: Regular Visits:
- Scheduled follow-ups for adjustments, monitoring, and imaging.
- Fixator Removal: Once consolidation is complete, a minor surgical procedure is performed to remove the external fixator.
Risks and Complications:
- Infection: At the pin or wire sites.
- Delayed Union or Nonunion: Slow or failed bone healing.
- Pin or Wire Loosening: This can lead to instability and potential complications.
- Nerve or Vessel Injury: Possible damage to surrounding nerves or blood vessels.
- Joint Stiffness: Due to prolonged immobilization or reduced activity.
Advantages
- Precision: Allows for gradual and precise correction, accommodating complex and severe deformities.
- Adaptability: Adjustments can be made in response to the bone’s healing and the body’s response to the correction process.
Gradual deformity correction is a highly effective method for treating complex orthopedic conditions. It requires a multidisciplinary approach involving orthopedic surgeons, physical therapists, and often specialists in radiology and rehabilitation to ensure the best outcomes for the patient.
For more information talk to a healthcare provider.
If you have any questions about Deformity Correction, please feel free and leave a comment.
Do share this blog with your friends and family!