WHAT’S A ROTATOR CUFF TEAR?
The rotator cuff tendons of the shoulder are very susceptible to gradual “atraumatic” tears over time from repetitive use, and acute “traumatic” tears that can occur from a sudden, violent force imparted onto the shoulder, like from a fall or while playing sports. When the rotator cuff is torn, it is often painful, particularly if the tear is traumatic. Rotator cuff tears can also cause biomechanical dysfunction, leading to an inability to elevate the shoulder.
Whether a tear develops suddenly or gradually, it can cause significant pain and limit your ability to move your shoulder. Typical symptoms include:
Common Symptoms of a Rotator Cuff Tear
Whether a tear develops suddenly or gradually, it can cause significant pain and limit your ability to move your shoulder. Typical symptoms include:
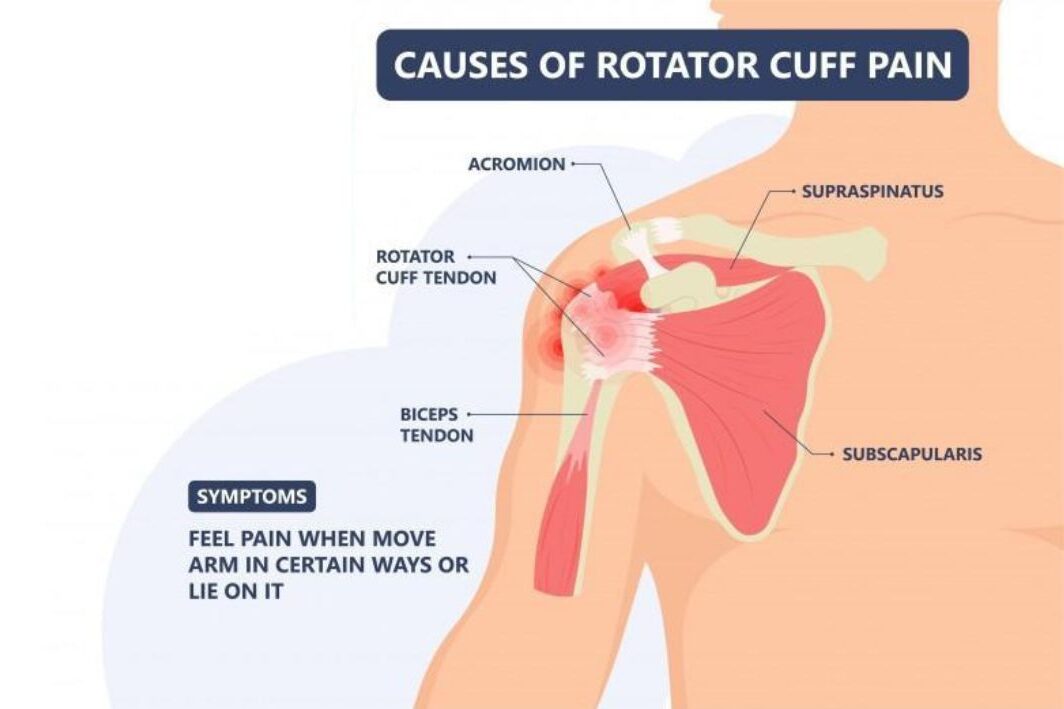
- Pain at rest or during certain movements
- Pain that interrupts sleep, especially when lying on the affected side
- Weakness when lifting or rotating your arm
- A crackling or popping sensation with movement
- Sudden, intense pain after an injury — sometimes accompanied by a snapping sound
With chronic tears, discomfort often worsens over time. Tasks like combing your hair, brushing your teeth, or reaching overhead can become painful or nearly impossible.
CHRONIC ROTATOR CUFF TEARS
Over time, the rotator cuff can begin to degenerate — especially after the age of 40. “Chronic” or “atraumatic” tears typically develop gradually due to repetitive use, wear and tear, or decreased blood flow to the tendons.
Common causes include:
- Bone Spurs: As we age, small bone overgrowths can form on the acromion bone. These spurs can rub against the rotator cuff tendons, leading to tears.
- Repetitive Motion: Overhead activities in sports (like baseball, tennis, or swimming) or jobs involving heavy lifting can stress the tendons.
- Decreased Blood Supply: Aging reduces blood flow to the tendons, slowing the body’s natural repair process.
ACUTE ROTATOR CUFF TEARS
Unlike chronic tears, acute rotator cuff injuries happen suddenly — often during a fall, while lifting something heavy, or from a quick, jerking motion. These injuries can occur alone or alongside other shoulder trauma, such as a dislocation or collarbone fracture.
A minor acute tear may heal within six to eight weeks, but severe tears may require medical treatment or even surgery to restore proper function.
For more information, talk to a healthcare provider.
If you have any questions about ROTATOR CUFF TEAR, Please feel free to leave a comment.
Do share this blog with your friends and family!





